
Andre Coelho/EPA/AAP
Sunit K. Singh, Banaras Hindu UniversityOver a year into the pandemic, questions around immune responses after COVID continue to confound.
One question many people are asking is whether the immunity you get from contracting COVID and recovering is enough to protect you in the future.
The answer is no, it’s not.
Here’s why.
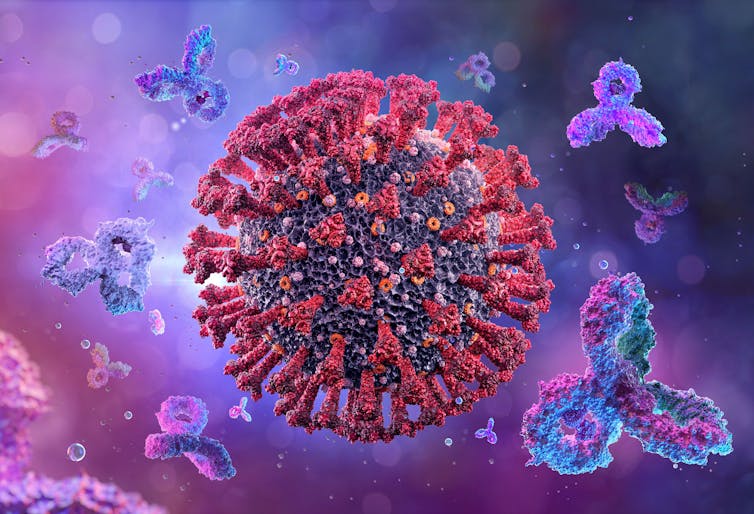
Remind me, how does our immune response work?
Immune responses are innate or acquired. Innate, or short-term immunity, occurs when immune cells that are the body’s first line of defence are activated against a pathogen like a virus or bacteria.
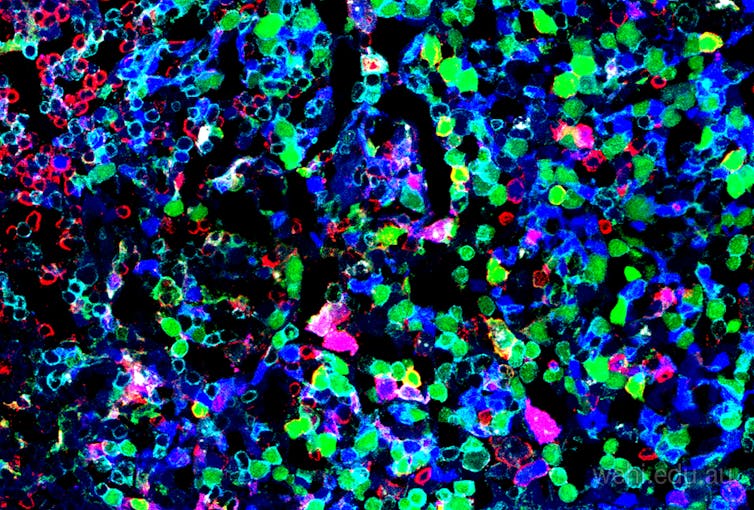
If the pathogen is able to cross the first line of defence, T-cells and B-cells are triggered into action. B-cells fight through secreted proteins called antibodies, specific to each pathogen. T-cells can be categorised into helper T-cells and killer T-cells. Helper T-cells “help” B-cells in making antibodies. Killer T-cells directly kill infected cells.
Once the battle is over, B-cells and T-cells develop “memory” and can recognise the invading pathogen next time. This is known as acquired or adaptive immunity, which triggers long-term protection.
What happens when you get reinfected? Memory B-cells don’t just produce identical antibodies, they also produce antibody variants. These diverse set of antibodies form an elaborate security ring to fight SARS-CoV-2 variants.
Natural immunity is not enough
Getting COVID and recovering (known as “natural infection”) doesn’t appear to generate protection as robust as that generated after vaccination.
And the immune response generated post-infection and vaccination, known as hybrid immunity, is more potent than either natural infection or vaccination alone.
People who have had COVID and recovered and then been vaccinated against COVID have more diverse and high-quality memory B-cell responses than people who’ve just been vaccinated.
Studies indicate mRNA vaccines generate a more potent immune response with previous infection, at least against some variants including Alpha and Beta.
And studies have shown that antibody levels were higher among those who’d recovered from COVID and were subsequently vaccinated than those who’d only had the infection.
Memory B-cells against the coronavirus have been reported to be five to ten times higher in people vaccinated post-infection than natural infection or vaccination alone.
Is one dose enough after COVID?
Some reports have suggested people who’ve had COVID need only one dose of the vaccine. Clinical trials of approved vaccines didn’t generate relevant data because people who’d already had COVID were excluded from phase 3 trials.
One study from June showed people with previous exposure to SARS-CoV-2 tended to mount powerful immune responses to a single mRNA shot. They didn’t gain much benefit from a second jab.
A single dose of an mRNA vaccine after infection achieves similar levels of antibodies against the spike protein’s receptor binding domain (which allows the virus to attach to our cells) compared to double doses of vaccination in people never exposed to SARS-CoV-2.
We need more studies to fully understand how long memory B-cell and T-cell responses will last in both groups.
Also, a single dose strategy has only been studied for mRNA-based vaccines. More data is required to understand whether one jab post-infection would be effective for all the vaccines.
At this stage, it’s still good to have both doses of a COVID vaccine after recovering from COVID.
Does Delta change things?
The development of new vaccines must keep pace with the evolution of the coronavirus.
At least one variant seems to have evolved enough to overtake others, Delta, which is about 60% more transmissible than the Alpha variant. Delta is moderately resistant to vaccines, meaning it can reduce how well the vaccines work, particularly in people who’ve only had one dose.
There’s no data available yet about how effective a single jab is for people who were previously infected with Delta and recovered.
The most important thing you can do to protect yourself from Delta is to get fully vaccinated.
According to a Public Health England report, one dose of Pfizer offered only about 33% protection against symptomatic disease with Delta, but two doses was 88% effective. Two doses was also 96% effective against hospitalisation from Delta. The AstraZeneca vaccine was 92% effective against hospitalisation from Delta after two doses.
A few vaccine manufacturers, including Pfizer, are now planning to use a potential third dose as a booster to combat the Delta variant.![]()
Sunit K. Singh, Professor of Molecular Immunology and Virology, Institute of Medical Sciences, Banaras Hindu University
This article is republished from The Conversation under a Creative Commons license. Read the original article.






















You must be logged in to post a comment.